Drug Distribution
انتشار الدواء و بيعرف على انه عملية انتشار الدواء من
الدم الى الخلايا و العكس والعملية دى بتعتمد على
1- capillary
permeability
ودى فيها نقطتين اول نقطة تركيب الشعيرة الدموىة وتانى
نقطة اللطبيعه الكيميائية للدواء
الشعيرة بيبقى فيها basement membrane محاط بطبقة من indothelial cell الطبقة دى بيبقى فيها فتحات اسمها slit junctions فبالتالى بيبقى فى جزء من ال basement membrane ظاهر(الجزء الظاهر ده بيختلف
من شعيرة دموية لشعيرة أخرى حسب مكان وجودها فى الجسم )المهم ان الجزء الظاهر ده
هو اللى بيمر منه الplasma
proteins ، لكن فال brain مفيش
slit junctions
وفى طبقة سميكة من
الدهون فبالتالى lipid drugs هتمر لل brain لكن ال charged
drugs مش هتعرف تمر ولازم تدخل على carriers بال Active
transport
تانى عامل بيأثر على الانتشار هو
2- blood flow لانه بيختلف
من مكان لمكان لان ال Cardiac output بيختلف من عضو لعضو يعنى مثلا بيبقى كتير للكبد
والكلية و المخ لكن بيبقى قليل للخلايا الدهنيه والجلد وهكذا.
تالت عامل بقى هو درجة ارتباط الدواء ببروتينات الدم
3- the degree of
binding of the drug to plasma proteins
الالبيومين هو اكتر بروتين بترتبط بيه الادوية لدرجة انه
ممكن يكون مخزن للدواء ( لما كمية الدواء الغير مرتبطة ببروتينات تقل بسبب تكسيره
فالكبد او اخراجه يروح الالبيومين مطلع شوية
هنتكلم بقى دلوقت عن حاجه اسمها
-volume of
distribution
وهو عبارة عن النسبه بين كمية الدواء اللى دخلت جسمنا
وتركيز الدواء اللى وصل للبلازما وبتتحسب بالمعادلة دى
( Amount
of drug in the body ( Q
------------------------------ = volume of distribution Vd
( Plasma drug concentration ( C
large molecular weight
drugs- بترتبط ببروتينات البلازما وبالتالى بتنتشر
فالبلازما بس اللى هى حوالى 6% من وزن الجسم يعنى 4 ليتر فى شخص
وزنه 70 كيلو
low molecular weight hydrophilic drugs- بتقدر تعدى من ال slit gunction وتوصل لل extracellular fluid لكن مش
بتقدر توصل لل intracellular
fluid وبالتالى بتنتشر فى حجم ( البلازما + السوائل
اللى خارج الخلية )
بيكون تقريبا 20 % من وزن الجسم يعنى 14
ليتر فى شخص وزنه 70 كيلو
low molecular weight hydrophobic drugs- بتقدر تعدى
وتدخل جوة الخلية يبقى هتكون منتشرة فالبلازما والسوائل خارج الخلية والسوائل داخل
الخلية (كل سوائل الجسم )يعنى تقريبا 60 % من وزن الجسم تقريبا 42 ليتر فى شخص
وزنه 70 كيلو
- فى الحوامل ال Vd بيزيد فى حالة الادوية اللى هى extremely lipid soluble لانه بينتشر وبيوصل الplacenta .
-فى بعض الاحيان بيبقى عندنا دواء مثلا (2) بيبقى مرتبط
ببروتينات البلازما وناخد دواء تانى
هنسميه (1) ييجى بقى الدواء رقم(1 ) ياخد
مكان الدواء (2) على البروتين ويخلى الدواء (1) حر فالدم وبالتالى تركيزه هيزيد
وممكن يوصل لل toxic concentration
طيب نشوف أمثله على كده
1-Chloral hydrate
,clofibrate ,phenybutazone can displace coumarin which is anticoagulant
,وبالتالى لو خدنا اى دواء من التلاته دول مع
الcoumarin هيحصل نزيف.
2-Salicylates
can displace Tolbutamide which is a hypoglycemic drug يعنى
هيحصل غيبوبة سكر لو خدنا النوعين دول مع بعض
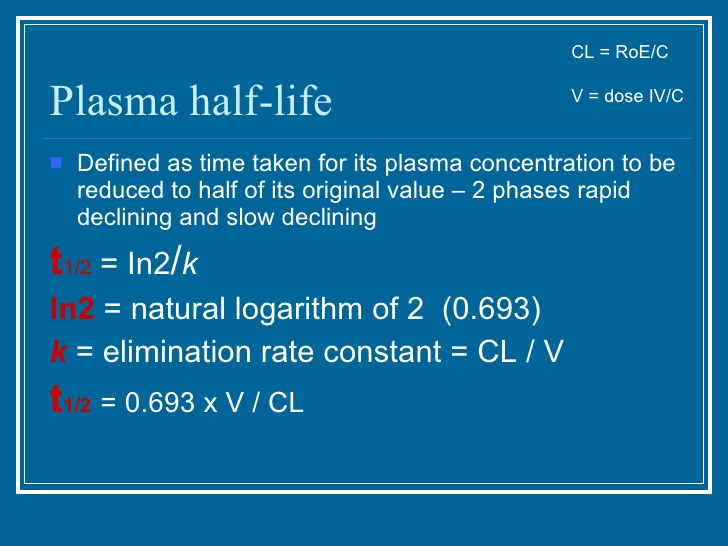
- لما بيكون Vd كبيرة بيبقى الhalf-life
بتاعة الدواء عاليه واى عامل بيزود ال Vd اكيد
هيزود ال half-life
بتاعة الدواء.
4- the degree of
binding of the drug to tissue proteins.
رابع عامل بيأثر على انتشار الدواء هو درجة ارتباط
الدواء ببروتينات الخلية لان بعض الادوية بتفضل تتجمع فى بعض الخلايا مثلا
Chlorpromazine prefer Brain
Digitoxin prefer Liver ,Kidney & Heart
Tetracycline prefer Bones & Teeth
Calcium prefer Collagen
Arsenic prefer Keratin
Iodine prefer Thyroid gland .... and so on
خامس حاجه بقى بتأثر على الانتشار هى
5- hydrophobicity
of the or drug structure
Hydrophobic drugs (lipophilic drugs)
بتقدر تمر من اى جدار وتدخل جوة الخلية لكن ده بيعتمد على ال blood flow لمنطقة الانتشار
لكن hydrophilic drugs مش بتقدر تدوب فى جدار الخلية الدهنى عشان تدخل الخلية ، لكن ممكن تمر
من ال slit junctions .